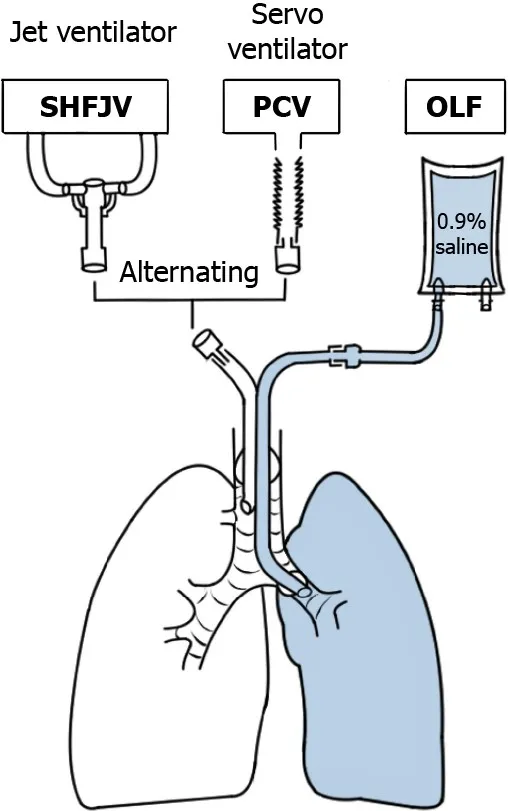
Servo Pressure on Jet Ventilator: Principles and Clinical Applications
High-frequency jet ventilation (HFJV) represents a specialized mode of mechanical ventilation that delivers small tidal volumes at very high frequencies (typically 100-600 breaths per minute). At the heart of its precise and safe operation lies a key parameter: servo pressure. Unlike conventional ventilators that rely primarily on set tidal volumes or pressures, jet ventilators use servo pressure as a fundamental control variable to govern the driving force behind each high-velocity jet pulse. This article delves into the principles, clinical significance, and optimization of servo pressure in jet ventilation.
Core Concept Overview
Servo pressure, often displayed in units of pounds per square inch (psi) or bar, is the regulated driving pressure supplied to the jet ventilator's solenoid valve. It directly determines the kinetic energy of the gas jet injected into the patient's airway. This pressure is meticulously controlled by a servo-regulator within the ventilator to maintain consistency despite fluctuations in gas supply or downstream resistance.
The Physiological and Mechanical Role of Servo Pressure
Servo pressure is not the pressure delivered to the alveoli; rather, it is the upstream driving pressure. Its primary function is to ensure a consistent and adjustable inspiratory flow and volume, which is critical given the very short inspiratory times (often 20-40 milliseconds) in HFJV.
1. Determinant of Tidal Volume Delivery
The most direct relationship of servo pressure is with the delivered tidal volume. A higher servo pressure generates a higher velocity jet, entraining more ambient air (the Bernoulli effect), resulting in a larger tidal volume. Clinicians titrate servo pressure to achieve adequate chest wiggle and carbon dioxide elimination.
2. Compensation for Airway Resistance and Compliance Changes
The servo-control mechanism dynamically adjusts to maintain the set pressure at the valve. If resistance increases (e.g., from kinked tubing or secretions), the system compensates to maintain the jet's driving force, promoting more stable ventilation than a simple fixed-pressure source.
3. Safety and Barotrauma Prevention
By precisely controlling the driving pressure, servo regulation inherently limits the maximum energy transferred to the airways. This is a vital safety feature, helping to mitigate the risk of barotrauma and volutrauma, which are concerns in conventional ventilation, especially in stiff lungs.
Clinical Applications and Servo Pressure Adjustment
Optimal servo pressure varies widely based on clinical context, patient size, and lung pathology. The following table outlines general guidance for servo pressure settings across different scenarios:
| Clinical Scenario | Typical Servo Pressure Range (PSI) | Clinical Objective | Monitoring Focus |
|---|---|---|---|
| Adult Laryngeal Surgery | 15 - 25 PSI | Provide adequate gas exchange while minimizing airway movement for surgical precision. | SpO₂, EtCO₂ waveform, chest excursion. |
| Neonatal/Pediatric Respiratory Failure | 8 - 15 PSI | Deliver ultra-low tidal volumes to prevent ventilator-induced lung injury. | Blood gases, chest wiggle, mean airway pressure. |
| Bronchopleural Fistula Management | 10 - 20 PSI | Reduce mean airway pressure and tidal volume to decrease air leak. | Air leak measurement, PaCO₂, hemodynamics. |
| ICU Rescue Therapy for ARDS | 20 - 35 PSI | Improve oxygenation and CO₂ clearance in severe restrictive disease. | PaO₂/FiO₂ ratio, compliance, hemodynamics. |
Initial Setup and Titration
Setup begins with a low servo pressure (e.g., 10-15 psi in adults). It is then incrementally increased while monitoring chest rise ("chest wiggle"), end-tidal CO₂, and oxygenation. The goal is to use the lowest effective servo pressure that achieves acceptable gas exchange, thereby minimizing dynamic hyperinflation and cardiovascular effects.
Technical Considerations and Limitations
Interaction with Other Parameters
Servo pressure does not act in isolation. Its effect is modulated by:
- Inspiratory Time (Ti): A longer Ti at a given servo pressure delivers a larger volume.
- Frequency (f): Higher frequencies reduce time for expiration, potentially leading to air trapping. Servo pressure may need reduction at very high f.
- FiO₂: The jet gas is 100% O₂, but entrained air dilutes it. Higher servo pressure increases entrainment, which can paradoxically lower delivered FiO₂.
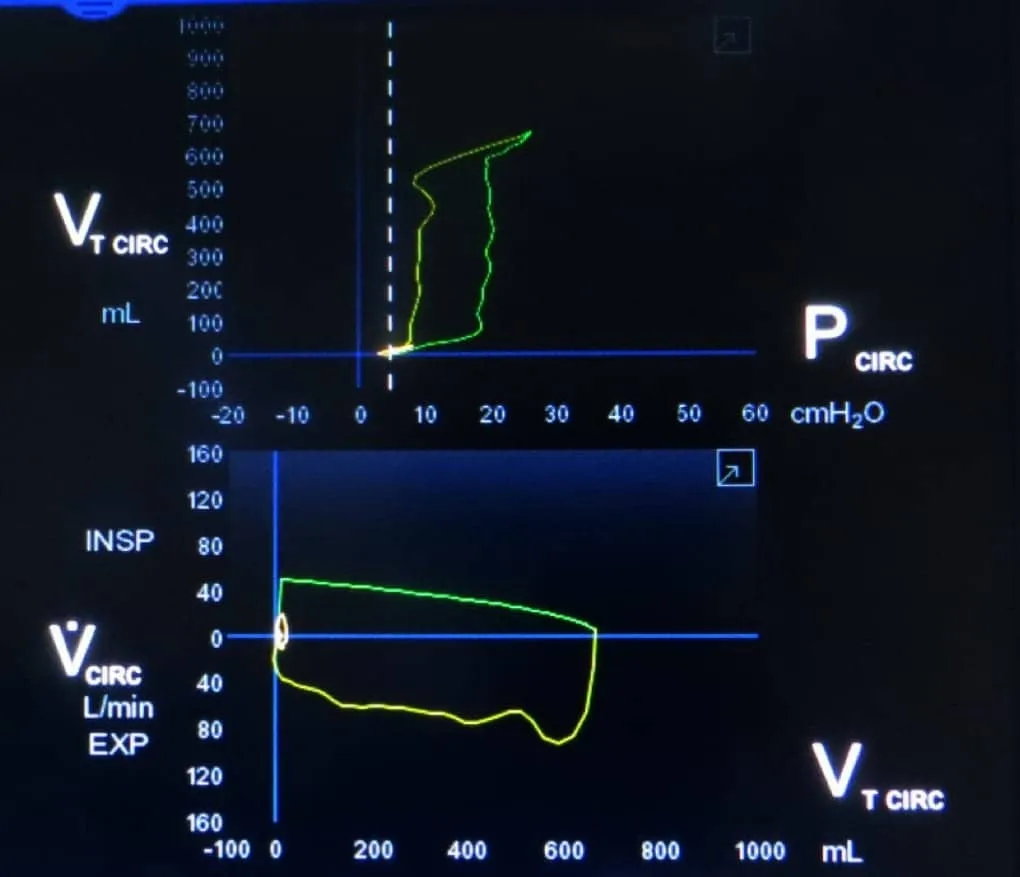
Monitoring Challenges
Direct measurement of delivered tidal volume is difficult in HFJV. Therefore, clinicians rely on surrogate markers like chest wiggle, arterial blood gases, and especially transcutaneous or end-tidal CO₂ monitoring, making servo pressure titration an indirect and skill-dependent process.
Conclusion: The Central Role of a Precise Control Variable
Servo pressure is the cornerstone of controlled and safe high-frequency jet ventilation. It transforms a raw high-pressure gas source into a finely tuned physiological tool. Understanding its role as the primary determinant of jet energy and tidal volume is essential for any clinician operating or managing patients on jet ventilators. Mastery of servo pressure adjustment, in concert with other parameters, allows this unique mode of ventilation to fulfill its potential in providing effective gas exchange in some of the most challenging clinical situations, from the operating room to the intensive care unit.